Breast cancer and cyst formation are at epidemic proportions. At what point can we say, conclusively, that aluminum in antiperspirants is causal? The evidence grows stronger and stronger, largely due to the labors of one dedicated scientist, but she states that absolute proof does not yet exist. So, how much proof do you require before deciding it’s better to be safe than sorry?
by Heidi Stevenson
Antiperspirants: Cause of Breast Cancer? discussed some of Keele Conference scientist Philippa Darbre’s work on the likelihood of a relationship between aluminum in antiperspirants and breast cancer, in particular locations of aluminum in breast tissue and aluminum as an estrogen mimic. This article follows her work into other areas as the noose tightens around antiperspirant aluminum as a serious risk in breast diseases.
As previously noted in Antiperspirants: Cause of Breast Cancer?, Dr. Philippa Darbre’s latest presentation at the Keele Conference was on research demonstrating the ability of aluminum to cause changes in proteins that may lead to cancer metastasis, which can turn a benign tumor into a malignant metastatic cancer. Here is information she’s elicited in earlier work that has led to the study on aluminum’s potential to cause breast cancer metastasis.
Aluminum’s Interference with Iron Homeostasis
As noted in the previous report, aluminum is found in the breasts of women with breast cancer and it’s more prevalent in the region where the majority of cancers occur. Though too much iron is toxic, some is required for health. Transferrin binds iron in body fluids, and ferritin holds onto iron in cells, releasing it as needed. Aluminum can interfere with the function of ferritin and transferrin, thus destabilizing iron homeostasis.
Dr. Darbre worked with Professor Ferdinando Mannello on aluminum content in nipple aspirate fluid (which is exactly what it sounds like). They and the rest of their team obtained nipple aspirate fluid from both women with and without cancer, and examined it for levels of ferritin and transferrin.[1] They withdrew nipple aspirate fluid (NAF) from the breasts of 16 women without cancer and 19 with cancer. Here’s a table of their results:
 First, notice that the amount of aluminum in NAF from cancerous breasts is more than double that of non-cancerous breasts! (268.4 µg/L / 131.3 µg/L) Notice also that ferritin is about five times higher in cancerous breasts (280.0 µg/L / 55.5 µg/L), and transferrin is almost 3 times higher (8.3 µg/L / 28 µg/L).
First, notice that the amount of aluminum in NAF from cancerous breasts is more than double that of non-cancerous breasts! (268.4 µg/L / 131.3 µg/L) Notice also that ferritin is about five times higher in cancerous breasts (280.0 µg/L / 55.5 µg/L), and transferrin is almost 3 times higher (8.3 µg/L / 28 µg/L).
 Milk levels of aluminum are greater than serum levels. That’s very important for nursing mothers to know, so that they can try to find ways ot lessening their aluminum load.
Milk levels of aluminum are greater than serum levels. That’s very important for nursing mothers to know, so that they can try to find ways ot lessening their aluminum load.
You can see the relative comparison in aluminum, ferritin, and transferrin between cancerous and noncancerous breasts in the bar graph. (Note that a separate graph is used for transferrin because there’s so much less of it that the difference wouldn’t be obvious on the scale used for aluminum and ferritin.)
 The scattergraphs to the left definitively demonstrate a genuine connection between aluminum and both ferritin and transferrin. To see if a correlation exists between two sets of points, simply plotting them on a graph is fairly straightforward. If there is a relationship, then you can generally see the points arranging around a line, as you can clearly see is true for aluminum and ferritin in cancer patients (top left graph), and also for aluminum and transferrin in cancer patients.
The scattergraphs to the left definitively demonstrate a genuine connection between aluminum and both ferritin and transferrin. To see if a correlation exists between two sets of points, simply plotting them on a graph is fairly straightforward. If there is a relationship, then you can generally see the points arranging around a line, as you can clearly see is true for aluminum and ferritin in cancer patients (top left graph), and also for aluminum and transferrin in cancer patients.
However, if you look at the bottom two graphs, it’s quite clear that there is no correlation between aluminum and either ferritin or transferrin in non-cancerous patients.
Aluminum’s Association with Breast Cysts
A common problem in women is gross cystic breast disease. Though generally considered benign, it can be quite painful and results in a huge number of doctor visits for treatment, usually by aspiration or, in extreme cases, surgical removal. Occasionally, these cysts can mimic cancer, resulting in testing, biopsies, and worry. These cysts are divided into two types: Type I are more likely to develop into more severe pathologies—meaning cancer—than type II cysts. Women who suffer from type I cysts are more likely to develop them frequently and in large numbers.
Philippa Darbre investigated the potential association between antiperspirant aluminum and gross cystic breast disease.[2] The report on the study states:
On the basis that antiperspirant formulations are designed to block apocrine sweat ducts of the axilla, and breast cysts result from blocked breast ducts, it has recently been hypothesized that breast cysts might also arise from antiperspirant use.
 Darbre and associates examined breast cyst fluid (BCF) from 48 samples, 27 of type I and 21 of type II. These results were compared with samples from blood sera and milk. Result averages are shown in this table published from the study.
Darbre and associates examined breast cyst fluid (BCF) from 48 samples, 27 of type I and 21 of type II. These results were compared with samples from blood sera and milk. Result averages are shown in this table published from the study.
The average amount of aluminum found in breast cyst fluid (BCF) was 90.0 µg/L, with 150.0 µg/L in type I cysts (the more cancer-prone type) and 32.0 µg/L in type II cysts. Notice that the amounts of aluminum found in blood sera, healthy and non-cancerous breast tissue in cancerous breasts (GCBD-matched) was significantly lower than found in either type I or II cyst.
Aluminum levels found in general milk samples and specific types of milk (colostrum, intermediate, and mature) are much higher than in healthy or non-cancerous tissues. This might be of serious concern to nursing mothers, as it indicates high levels of aluminum in their breast milk, irregardless of whether they suffer from cystic breast disease.
 The amount of aluminum found in both cyst types is dramatically greater than in normal tissues or milk, but particularly notable is that the more cancer-prone breast cysts have extremely high levels of aluminum, averaging about 150.0 µg/L. The graph to the left makes this easy to see. Note, also, that there is no overlap between the lowest amount of aluminum found in type I breast cysts and the greatest amount found in type II breast cysts. Also note that, in the table above, the p-value is less than .0001, indicating that there is almost no likelihood that the results were obtained by chance.
The amount of aluminum found in both cyst types is dramatically greater than in normal tissues or milk, but particularly notable is that the more cancer-prone breast cysts have extremely high levels of aluminum, averaging about 150.0 µg/L. The graph to the left makes this easy to see. Note, also, that there is no overlap between the lowest amount of aluminum found in type I breast cysts and the greatest amount found in type II breast cysts. Also note that, in the table above, the p-value is less than .0001, indicating that there is almost no likelihood that the results were obtained by chance.
Do Antiperspirants Cause Breast Cancer?
Writing for Elsevier’s Encyclopedia of Environmental Health 1st Edition, Dr. Philippa Darbre discusses the fact that more and more breast cancer is found in the upper outer quadrant (UOQ) of the breast.[3] Although it had been suggested that this might be a result of weight gains, the facts don’t fit that idea. She wrote:
Numerous clinical studies dating back to the 1920s have shown that the UOQ of the breast is the most frequent site of carcinoma, but strangely the relative proportion
of breast cancer in the UOQ appears to rise chronologically with the year of publication.
She presented the following graphs to help explain:

The relative incidence of breast cancer in the upper outer quadrant (UOQ) of the breast, as reported in the scientific
literature, appears to rise chronologically with year of publication from 1928 to 1994. Using a single study population of England and Wales, the relative percentage of UOQ breast cancer has risen annually on a linear basis between 1979 and 2000, and in independent records in Scotland, a similar trend was noted between 1980 and 2001.
These graphs are pointing out that the relative rate of increase in cancer of the upper outer quadrant keeps increasing at a linear rate, year after year, in comparison to all other breast cancer locations. The top bar shows this in terms of publications that have reported on the phenomenon since 1928, when UOQ cancers were 30.9% of all breast cancers, but had reached 60.7% in 1994. Fat cannot be to blame for the increase in UOQ cancers, because it cannot explain why it would increase so consistently relative to other breast cancer locations.
There are certainly other carcinogenic chemicals in the environment that could be playing a factor in breast cancer increases. Dr. Darbre discusses them, including parabens, bisphenol A, phthalates, polycyclic musks, triclosan, and ultraviolet light filters (sun screen lotions and cosmetics). However, the amount of aluminum found in antiperspirants is very high, and it’s applied on and next to breast tissue and in the area of the greatest increase in cancer, the upper outer quadrant.
Furthermore, aluminum in antiperspirants is left on the skin and is absorbed through the skin. Antiperspirants work by combining with wastes in perspiration ducts, thus plugging them, limiting detoxification capability.
Dr. Darbre’s still unpublished study presented at the last Keele Conference demonstrates that aluminum has the ability to create changes in breast tumors, making them metastasize. It stands in addition to an already extensive body of work building the case of antiperspirants’ adverse effects. She is, though, the first to clarify that a cause and effect connection between antiperspirants and breast cancer has not yet been demonstrated. Nonetheless, her research keeps drawing the noose tighter.
The question you must answer is: How absolute must the proof be before you want to take action to prevent potential harm from a product, especially one that is not necessary for life? It’s quite obvious that our regulatory agencies are not moving to protect us, though the odds of a woman developing breast cancer are now about 1 in 8—and more and more men are also developing it.
Surely the precautionary principle says that the information now available on an association between antiperspirant aluminum and breast cancer is far more than required to stop using antiperspirants until shown to be safe. It is, though, up to you to decide how much risk you’re willing to accept.
Sources:
- Analysis of aluminium content and iron homeostasis in nipple aspirate fluids from healthy women and breast cancer-affected patients; Journal of Applied Toxicology; Ferdinando Mannello, Gaetana A. Tonti, Virginia Medda, Patrizia Simone, Philippa D. Darbre; DOI: 10.1002/jat.1641
- Concentration of aluminium in breast cyst fluids collected from women affected by gross cystic breast disease; Journal of Applied Toxicology; Ferdinando Mannello,a Gaetana A. Tonti and Philippa D. Darbre; DOI: 10.1002/jat.1384
- Personal Care Products and Breast Cancer; Elsevier; Encyclopedia of Environmental Health 1st Edition; P. Darbre;

 They are reports from Germany showing, on the left, the number of TB mortalities from 1956-1988, and on the right, the number of reported cases from 1949-1987. The BCG vaccine against TB was introduced in 1970. (The area in the rectangles represents the total number of vaccinations given during the decade from 1970-1980.) It matters not whether you take a quick look or a long one, it’s obvious that the TB vaccination had absolutely nothing to do with the reduction in either cases of TB or deaths from it.
They are reports from Germany showing, on the left, the number of TB mortalities from 1956-1988, and on the right, the number of reported cases from 1949-1987. The BCG vaccine against TB was introduced in 1970. (The area in the rectangles represents the total number of vaccinations given during the decade from 1970-1980.) It matters not whether you take a quick look or a long one, it’s obvious that the TB vaccination had absolutely nothing to do with the reduction in either cases of TB or deaths from it. To the right is a graph of the pertussis (whooping cough) mortality rate from 1946-1987 in Germany, with the times that the original pertussis vaccine was introduced and the diphtheria-pertussis-tetanus vaccine took its place. As can be seen, the death rate from pertussis stayed on approximately the same downward trajectory it had been on at the time of vaccine implementation.
To the right is a graph of the pertussis (whooping cough) mortality rate from 1946-1987 in Germany, with the times that the original pertussis vaccine was introduced and the diphtheria-pertussis-tetanus vaccine took its place. As can be seen, the death rate from pertussis stayed on approximately the same downward trajectory it had been on at the time of vaccine implementation. The graph to the left shows the pertussis mortality rate in Switzerland from 1910-1980. The shaded area (at the top right of the graph) shows the introductory date of the pertussis vaccine in 1944, and shows how that vaccine’s coverage increased to nearly 100% by 1980. However, it is not possible to see any change in the trajectory of reduced pertussis deaths.
The graph to the left shows the pertussis mortality rate in Switzerland from 1910-1980. The shaded area (at the top right of the graph) shows the introductory date of the pertussis vaccine in 1944, and shows how that vaccine’s coverage increased to nearly 100% by 1980. However, it is not possible to see any change in the trajectory of reduced pertussis deaths. The next graph, shown to the right, shows the number of diphtheria deaths in Germany from 1920-1987. Notice that the diphtheria vaccine was introduced in 1925, with an enormous
The next graph, shown to the right, shows the number of diphtheria deaths in Germany from 1920-1987. Notice that the diphtheria vaccine was introduced in 1925, with an enormous 
 Autonomously-produced antibodies are called immunoglobulins. While the fetus starts to develop some immunoglobulin before birth, it takes time, in most instances more than a year, to reach maturity. The graph to the right shows the pace at which IgG from the mother increases and decreases, and the rate at which a neonate starts to produce its own, plus IgM, IgA, and IgD.
Autonomously-produced antibodies are called immunoglobulins. While the fetus starts to develop some immunoglobulin before birth, it takes time, in most instances more than a year, to reach maturity. The graph to the right shows the pace at which IgG from the mother increases and decreases, and the rate at which a neonate starts to produce its own, plus IgM, IgA, and IgD.

 Results are shown in the graph to the right. Both Al chloride and Al chlorhydrate interfere with breast cancer cell growth. Al chloride inhibited estradiol binding by 40% at 2.5 x molar excess (blue arrow) and 99.9% at 10 x molar excess (green circle). Al chlorhydrate inhibited estradiol binding by 64% at 5.0 x molar excess (red arrow) and 100% at 10 x molar excess (green circle).
Results are shown in the graph to the right. Both Al chloride and Al chlorhydrate interfere with breast cancer cell growth. Al chloride inhibited estradiol binding by 40% at 2.5 x molar excess (blue arrow) and 99.9% at 10 x molar excess (green circle). Al chlorhydrate inhibited estradiol binding by 64% at 5.0 x molar excess (red arrow) and 100% at 10 x molar excess (green circle). The next experiment is similar, but rather than investigating interference with estradiol function, the needed amount of Al chloride and Al chlorhydrate to interfere with breast cancer cell growth was investigated. MCF7 cancer cells were grown in the lab and then concentrations of Al chloride or Al chlorhydrate were introduced. A concentration of 10-3 mole of either Al chloride or Al chlorhydrate was required to cause disruption in cell growth. Therefore, MCF7 cells are resilient to high concentrations of these aluminum compounds.
The next experiment is similar, but rather than investigating interference with estradiol function, the needed amount of Al chloride and Al chlorhydrate to interfere with breast cancer cell growth was investigated. MCF7 cancer cells were grown in the lab and then concentrations of Al chloride or Al chlorhydrate were introduced. A concentration of 10-3 mole of either Al chloride or Al chlorhydrate was required to cause disruption in cell growth. Therefore, MCF7 cells are resilient to high concentrations of these aluminum compounds.


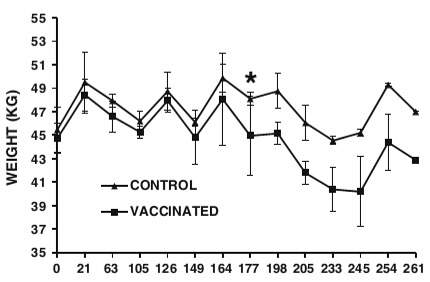
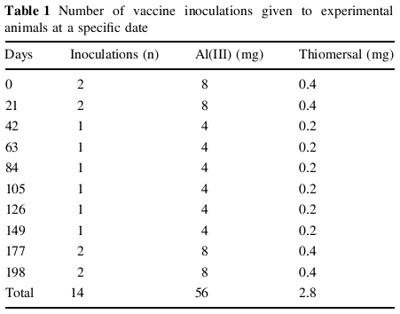 The researchers took 6 castrated 3-month old male lambs from an organic farm. They were divided into two groups of 3, one acting as controls remaining unvaccinated, and the other vaccinated according to the schedule on the right. The vaccines were for
The researchers took 6 castrated 3-month old male lambs from an organic farm. They were divided into two groups of 3, one acting as controls remaining unvaccinated, and the other vaccinated according to the schedule on the right. The vaccines were for